Introduction:
Many weed users wonder, does aspirin help pass a drug test? In this article, we will discuss the potential of aspirin for beating a drug test while describing how it can achieve this and looking at the opinions of users across social media. Aspirin is a medication designed to lessen fever, minor aches, pain, and inflammation. Some of its further applications include preventing blood clots as well as decreasing the chances of heart attacks and stroke.
Some marijuana users use aspirin in an attempt to pass a urinary drug test and less frequently in an effort to beat a hair follicle test. You should not take aspirin to pass a drug test if of course, you have an allergy to aspirin. You should also avoid taking aspirin for this purpose if you suffer a tendency to bleed, have active liver disease, have suffered from digestive tract problems in the recent past or if you are under the age of 21.
Aspirin should be taken with the consumption of large (but not unsafe) quantities of water. It is vitally important that you do not consume too much water or aspirin. Taking too much aspirin can be highly dangerous and possibly fatal. Lastly, trying any means to beat a drug test except abstinence may be illegal in your jurisdiction so look up your local laws on the matter.
 | Our #1 Choice Toxin Rid |
| |
 | Mega Clean + PreCleanse Pills |
|
Negative Side-Effects & Health Risks:
As with any medication, aspirin comes with a range of possible side effects and health risks.
Potential negative side effects of aspirin include; abdominal pains, bleeding, cramps, drowsy feelings, gastritis, gastrointestinal ulcers, headaches, heartburn, nausea, rash, and an upset stomach. Bleeding is a particularly notable health risk associated with aspirin and is thus why those with a tendency to bleed and other bleeding-related health problems should avoid taking aspirin to beat a drug test.
There is a risk that minor injuries or even old injuries could lead to significantly increased levels of bleeding than would occur otherwise if one is consuming aspirin at the time. Such bleeding can be external, internal or both.
Using Aspirin For A Drug Test
Does aspirin work to pass a drug test? Yes, it can if taken before an EMIT test. We will describe the methods here, but we are making no recommendations. The two most popular approaches that involve using aspirin to pass a urine test are as follows;
Method 1
- Consume roughly 1 liter of water over 2 hours.
- Four to six hours prior to the test, take 4 tablets of aspirin. Take each of these tablets over a spread out interval for health & safety purposes.
- Urinate at least twice prior to the test.
- You should collect the urine sample mid-stream when at the test facility.
Method 2
- Consume 2 aspirins roughly four to six hours before the test. Give at least half an hour intervals between each aspirin for health & safety purposes.
- Take 2 further aspirin tablets prior to the 2-hour mark before the test. Give at least half an hour intervals between each aspirin for health & safety purposes.
- Consume large quantities of water (albeit not unsafe amounts).
- Urinate several times before your test.
The aspirin tablets used in either method should be 325 mg each. Even spread out, taking this much aspirin is still substantial and should be done with caution. If you experience any negative side effects, seek medical support immediately.
Pros & Cons of These Methods
Next info given by FMAHealth. You might have many questions about this approach such as does aspirin show up on a drug test? If using aspirin for a urine drug test, you can be fairly sure they will not test for it.
Pros:
- Generally effective for an average, old-style EMIT urine drug test
- Cheap and easy to use
- Can work as a rapid preparation for a urinary drug test
- Usually safe once you follow the correct instructions
Cons:
- Risk of negative side effects including bleeding
- Aspirin can be detected in the sample
- Not suitable for everyone
- Requires the consumption of substantial quantities of water
- Largely limited to a urine drug test although may help to pass a hair follicle test
It has been scientific knowledge since at least 1994 (Wagener, Linder, and Valdes) that aspirin makes an EMIT or Enzyme Multiplied Immunoassay Technique which is a common and cheap urinary drug test more susceptible to false negatives. In this study, the ingestion of a common dose of aspirin had the effect of reducing the capacity of such drug tests to detect relevant toxins from a urine sample. The larger the dose taken by the subjects, the less able the testers were to detect drug residues in a sample.
However, it is vital to avoid the temptation of taking large doses of aspirin since this is not safe. Consuming too much aspirin can lead to serious health ramifications or/and death. The findings of the study infer that aspirin taken in responsible quantities is most likely to help with passing a cheap EMIT urine test but may not succeed in allowing you to pass more costly and complicated drug tests. Further, there is also a chance that the detection of aspirin in the sample by the testers may result in you failing the test or more likely being asked to retake the test.
 | Our #1 Choice Toxin Rid |
| |
 | Mega Clean + PreCleanse Pills |
|
Aspirin is not believed to have any direct effect on THC nor any other type of drug residue, but it does help to cloud the existence of drug toxins in a urine sample. Of course, consuming large quantities of water as part of a common aspirin pre-test method can in itself flush toxins from your body or dilute them.
It is important to be aware though that attempting to cheat on a drug test is illegal in some territories such as the U.S. states of Nebraska and Oklahoma. Be sure to research the laws of your region whether in the United States or elsewhere, in order to clarify that your actions are within the law.
Additional Information:
Does methocarbamol have aspirin in it? Methocarbamol is a medication used to treat muscle pain and spasms which does indeed contain aspirin. Most weed users avoid turning to this product to beat a drug test and if you are considering it, please do your research beforehand and ensure that any effort you are using to pass a drug test is safe and legal.
Social Media Reviews:
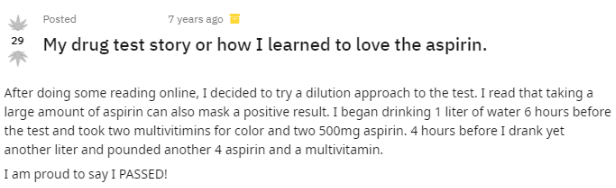
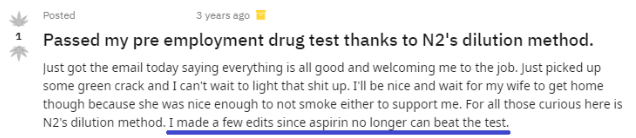
Positive Reviews:
Negative Reviews:
As you can see from the mix of positive and negative reviews featured above, aspirin is not guaranteed to work in beating a urine drug test.
Conclusion:
Can aspirin help pass a drug test? It has been scientific knowledge since the mid-1990s that aspirin can produce false-negatives for EMIT urine tests. There is also a range of claims from users across the internet that it has helped in passing hair follicle tests too although this is more speculation.
Detox drinks, synthetic urine, dilution, and substitution are arguably more reliable ways to beat a drug test. Further, with aspirin, you risk a list of potential side effects including bleeding and stomach ulcers. If you do however choose to use an aspirin method in an attempt to pass a drug test, do so with caution and best of luck!
Bibliography:
“News For Healthy, Older Patients: Toss Your Baby Aspirin.” Krumholz, Harlan, Forbes, 2018, https://www.forbes.com/sites/harlankrumholz/2018/09/17/news-for-healthy-older-patients-toss-your-baby-aspirin/
“Royalty-free blood test.” Pxfuel, Pxfuel, 2020, https://www.pxfuel.com/en/search?q=blood+test
“Passed a drug test in 8 days.” Grasscity, Grasscity, 2018, https://forum.grasscity.com/threads/passed-a-drug-test-in-8-days.1484732/
“My drug test story and how I learned to love the aspirin.” Reddit, Reddit, 2014,
https://www.reddit.com/r/trees/comments/r8ueu/my_drug_test_story_or_how_i_learned_to_love_the/
“Passed my pre-employment drug test thanks to N2’s dilution method.” Reddit, Reddit, 2018, https://www.reddit.com/r/trees/comments/4cmrkc/passed_my_pre_employment_drug_test_thanks_to_n2s/
“Does aspirin work to pass a drug test?” Daryl Seldon, FV KASA, 2019, https://www.fvkasa.org/english/health/detox/aspirin